MTHFR is well known for causing heart health issues. It’s directly responsible for raising homocysteine levels, it’s implicated in troublesome blood clotting, and it’s indirectly responsible for making it harder to make adequate nitric oxide.
All of this is compounded if you have MTHFR and another gene SNP called NOS3.
What is Nitric Oxide?
Nitric oxide is the primary substance responsible for keeping your blood vessels open and relaxed so that blood can flow through easily. Without it, your blood vessels tighten and constrict, which drives up blood pressure and reduces oxygenation of your tissues. The primary function of your blood is to carry oxygen to all of the muscles, organs, and tissues that need it, and nitric oxide helps make that happen.
Nitric oxide also helps to keep your platelets, those tiny flakes in your blood that make up blood clots, nice and smooth and slippery. It inhibits platelet aggregation and adhesion, and even helps to destabilize any small clots that have formed.
Blood that clots when you’re injured are a good thing – they keep you from losing too much blood. Blood clots that happen for no reason, are deadly. That is what lies underneath the bulk of the heart attacks and strokes out there. You want blood that is smooth and free of clots.
Nitric oxide also helps with the growth and formation of new blood vessels.
Why Does MTHFR Affect Nitric Oxide?
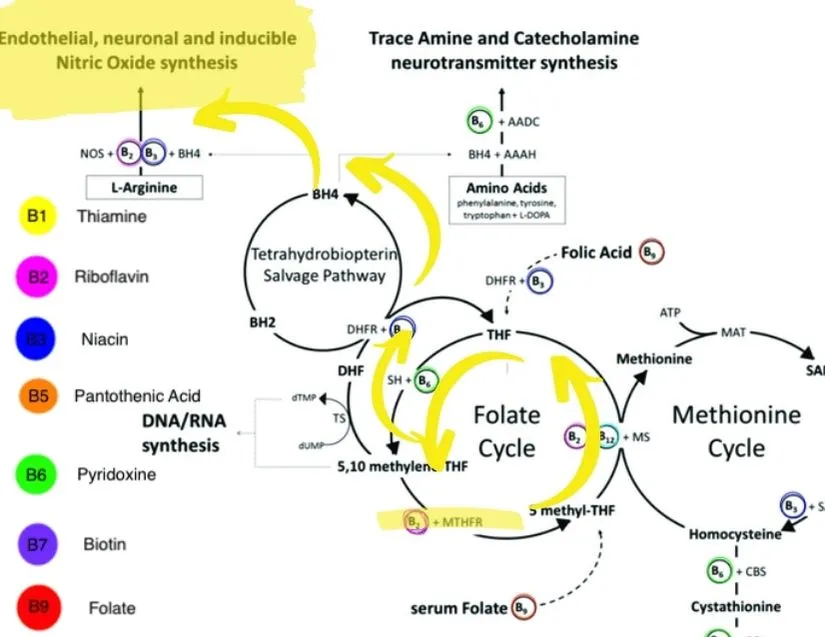
MTHFR is part of the folate cycle, turning inactive folate into the active form, which is 5-LMTHF. The folate cycle needs to spin in order for a linked pathway, the BH4 pathway, to also spin. The BH4 pathway is most known for neurotransmitter formation because this is where we see serotonin and dopamine formation. BH4 is also necessary for nitric oxide synthesis. There is a detailed pathway document in the show notes, if you really want to dive in, but suffice to say if MTHFR is sluggish, then nitric oxide synthesis is also sluggish.
Let’s Talk NOS
NOS stands for nitric oxide synthease and there are three different forms, depending on where they are located in your tissues. NOS1, is also called neuronal NOS (or nNOS). NOS2 is also called iNOS, or inducible NOS, and NOS3 is epithelial NOS, or eNOS. eNOS, or NOS3 is extremely important here because it is most represented in the epithelium, which lines your blood vessels and so has the greatest direct impact on vessel dilation as well as clotting.
Nitric oxide is made from arginine, which is one of the building blocks of protein, and so that matters for proper functioning, as does calcium. Under normal circumstances, NO synthesis is dependent on the level of calcium within the cell and so that must be adequate. NO synthesis can also be influenced by injuries, such as shear stress, that require changes to blood flow.
NOS “Uncoupling”
There are many factors, mostly implicated in heart disease, that can set up a bad situation with your NOS. These factors include diabetes, ongoing high blood pressure, high cholesterol, aging, and metabolic syndrome and they all lead to higher percentages of oxygen radicals, which can in turn cause NOS to break off of BH4, or “uncouple” and bond with a reactive oxygen species. This establishes a cascades of enhanced free radical production that does nobody any good. This is part of why your doctor is so eager to treat diabetes, high blood pressure, and cholesterol before they have a chance to do long-term damage.

NOS3 Gene SNP
The NOS3 gene SNP, as you might have guessed, has its biggest consequences in heart and cardiovascular health, but also influences some tissues that rely heavily on constant, tightly regulated blood flow like your brain or a developing fetus. It is especially likely to create problems in situations with overlapping pathology, like NOS3 Gene SNP with diabetes, which also decreases circulation.
Common signs of NOS3 problems:
- Chest pain with exertion or away from it
- Cold hands and feet (poor circulation)
- High blood pressure
- Erectile dysfunction
- Migraines
- Stroke
- Chronic sinus issues
- Blood clots
- Congenital heart defects (in babies born from mothers with untreated NOS3 polymorphisms)
- Arteriosclerosis or hardening of the arteries
- Preeclampsia in pregnancy (this is also a risk with MTHFR alone).
- Family or personal history of Alzheimer’s disease.
Supporting a NOS3 Polymorphism
There are many ways you can support nitric oxide synthesis in your body, with or without a NOS3 gene SNP. Here are just a few:
- Eliminate Folic Acid – folic acid causes a decrease in BH4, which is bad for your nitric oxide synthesis and your neurotransmitter production (also, your methylation).
- Hum! – eNOS is highly expressed in your sinuses, and humming causes a 15-20 x increase in nitric oxide synthesis in those tissues. This is part of why breathing through your nose at night is so important for tissue oxygenation. A wonderful study published in the journal Medical Hypothesis showed that not only will strong humming for an hour every evening clear up nasal blockages and sinus infections, it also increases your functional nitric oxide.
- Eat a low glycemic index diet – lowering your blood sugar fluctuations as well as your blood sugar in general will help your NOS, your heart, and your risk of diabetes in the long term. This means that every meal and snack should have a balance of proteins, good fats, fiber, complex carbs and sugars. A big pop or candy bar in the middle of the afternoon with no real food to back it up is the opposite of this.
- Breathe through your nose– talk with your doctor about mouth breathing (Especially at night), try mouth taping, and make sure any larger issues like deviated septum get addressed. Deep breathing exercises for one minute three times per day can really help as well.
- Exercise – exercise is great for everything and a healthy NOS3 is no exception.
- Stop smoking and stay away from chemicals – chemicals in your environment can impair your NOS function by reducing the amount of BH4 produced, as well as impacting glutathione levels and NOS needs support from glutathione so it doesn’t get into the uncoupling situation.
- Good dietary sources of arginine, calcium, and B2. Arginine comes from high protein foods like meat, dairy, and legumes which you will be eating more of with a low glycemic index diet. Calcium also comes from dairy, dark ark leafy greens, and broccoli. Riboflavin can be found in eggs, liver, lamb, mushrooms, spinach and almonds.
Whether you have a NOS3 polymorphisms or not, supporting a healthy nitric oxide function is crucial for a healthy heart, brain, and sinuses. It is especially important if you have an MTHFR polymorphism because we do have tendencies toward compromise in this area. Plus, most of the steps here overlap with the MTHFR lifestyle – so if you do the MTHFR lifestyle plus some deep breathing or humming, you’re there.
It’s important to note that the type of mutation and the number of copies you have, as well as the other genetic polymorphisms you may have, influence the health issues associated with MTHFR.
There are health issues or hazards if you just have one copy of the C677T or A1298C mutation.
The following conditions have been suggested to be linked to MTHFR:
- Blood clots, stroke, embolism, deep vein thrombosis, and heart attacks)
- Depression
- Anxiety
- Bipolar disorder
- Schizophrenia
- Increased risk for a variety of cancers
- Chronic leukemia
- Chronic fatigue and pain
- Nerve pain
- Migraine
- Repeat miscarriage
- Neural tube defects in babies
- Addiction
- Breast implant illness
- Increased risk for autoimmune conditions
Research on the effects of the MTHFR mutation in pregnancy is mixed, but there is a clearly increased risk of repeat miscarriages with MTHFR polymorphisms that is thought to be associated with microclotting. Studies are showing good results with either low dose aspirin thereapy alone, or low dose aspirin in combination with heparin to prevent pregnancy loss for women with MTHFR polymorphisms who have a history of repeat miscarriages.
Women with MTHFR polymorphisms also have increased risk of midline abnormalities including spina bifida, cleft lip, cleft palate, and anacephaly. These risks can be mitigated with appropriate supplementation with active folate and the other B vitamins necessary for nerual tube formation. Your fertility team should be informed if you have a known MTHFR polymorphism.
MTHFR is a common genetic mutation that can contribute to anxiety, depression, fatigue, chronic pain, infertility, and more serious conditions like breast implant illness, heart attack, stroke, chronic fatigue syndrome, and some types of cancer. If you know or suspect you have an MTHFR variant, schedule a free 15-minute meet-and-greet appointment with MTHFR expert Dr. Amy today.
Book Your Appointment

Thank you Amy. I have learned so much from you. I am so glad when I search for an answer, about my mthfr, that your article comes up. I have done most of your podcasts, and I get the Tuesday Tips. Thank you for sharing your knowledge and wisdom about mthfr. May you be continually blessed. CJ
Thanks so much, CJ!
If there is ever a topic you need to know about that I haven’t covered already, reach out!