This question seems to come up frequently in the MTHFR community, Genetic Rockstars. And of course, B12 levels have a lot to do with how you feel and how well you’re methylating on a daily basis, so it’s a really relevant conversation. Vitamin B12 is a cofactor in the recycling of homocysteine to methionine and in the generation of SAMe, which is the primary methyl donor, so it is something that every MTHFR mutant out there should be thinking about.
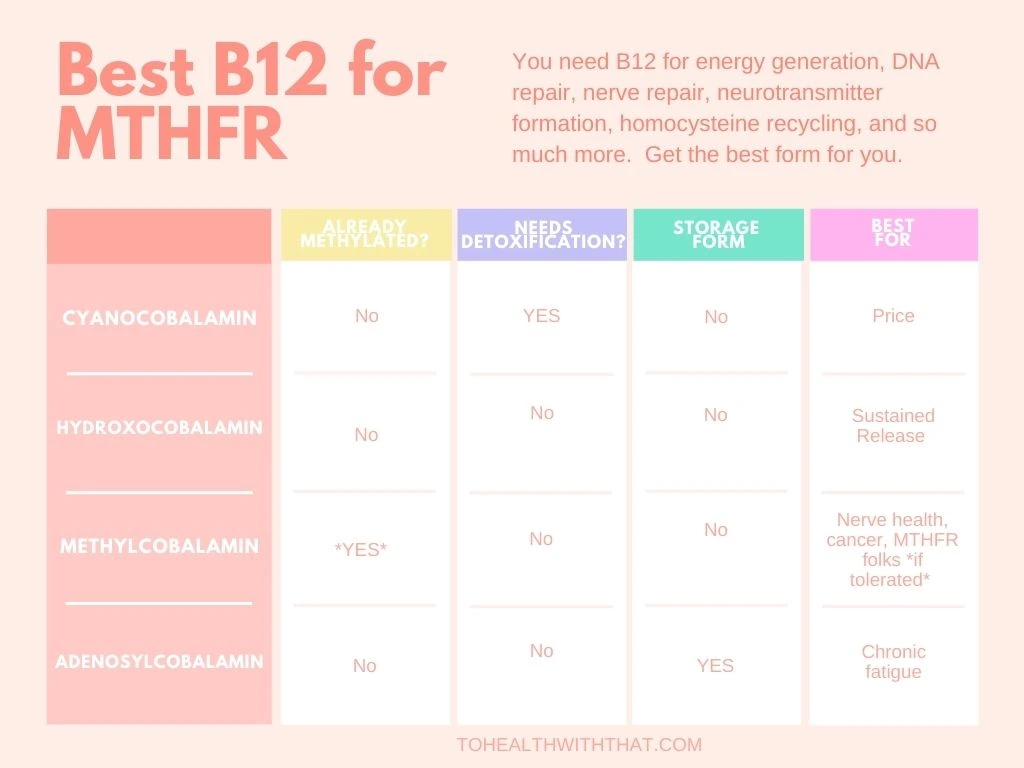
There are four commonly available forms of vitamin B12. The easiest to find and cheapest is cyanocobalamin, which is cobalamin, or B12, bonded to a cyanide carrier. Methyl B12 is the active form and needs no interconverting to be useful by the body. It is already bioavailable and active. HydroxoB12 is cobalamin bonded to a hydroxyl group, which is just oxygen and hydrogen and doesn’t require a lot of resources to detox. Adenosyl B12 is cobalamin carried by an adenosine, which is also useful in the body.
It seems really simple to say “of course, methyl is the best B12 for MTHFR folks – we have trouble methylating things and it’s already methylated, so this seems done and dusted.” And it is, for the most part. The issue is that in some cases, methyl B12 is too stimulating in the way that taking 5-LMTHF or methyl donors like TMG can be too stimulating. It’s just too quick a rush of too many good things at once and your body kind of freaks out. It’s technically “the best” but also can feel not so good. Let’s break down the forms one by one.

Cyanocobalamin
Cyanocobalamin is the cheapest to produce, cheapest to buy, most readily available, and easiest to store – it’s heat stable and resilient. It doesn’t absorb particularly well when taken orally and it does require a methyl group to convert into an active form. Also, your body has to actively detoxify the cyanide molecule. Cyanide has a big reputation as a toxin, but this is a very tiny dose. Also, absorption decreases if there are any compromises to stomach acid levels, which is a common problem in the Western world, as evidenced by the number of people taking medicines for reflux, heartburn, and the like.
For people with severely compromised methylation – like kids on the autism spectrum, symptoms can actually get worse, instead of better, with this form of B12 because it does require methylation and methyl groups are in such short supply.
Also, a small study that used radioactive markers on cyanocobalamin, showed that it takes more than 48 hours for cyanocobalamin to convert to methylcobalamin, which in terms of typical vitamin use, is extremely slow.
Overall, if there is no other source of B12 available then cyano is better than nothing, but if you have another choice, a different form is better.
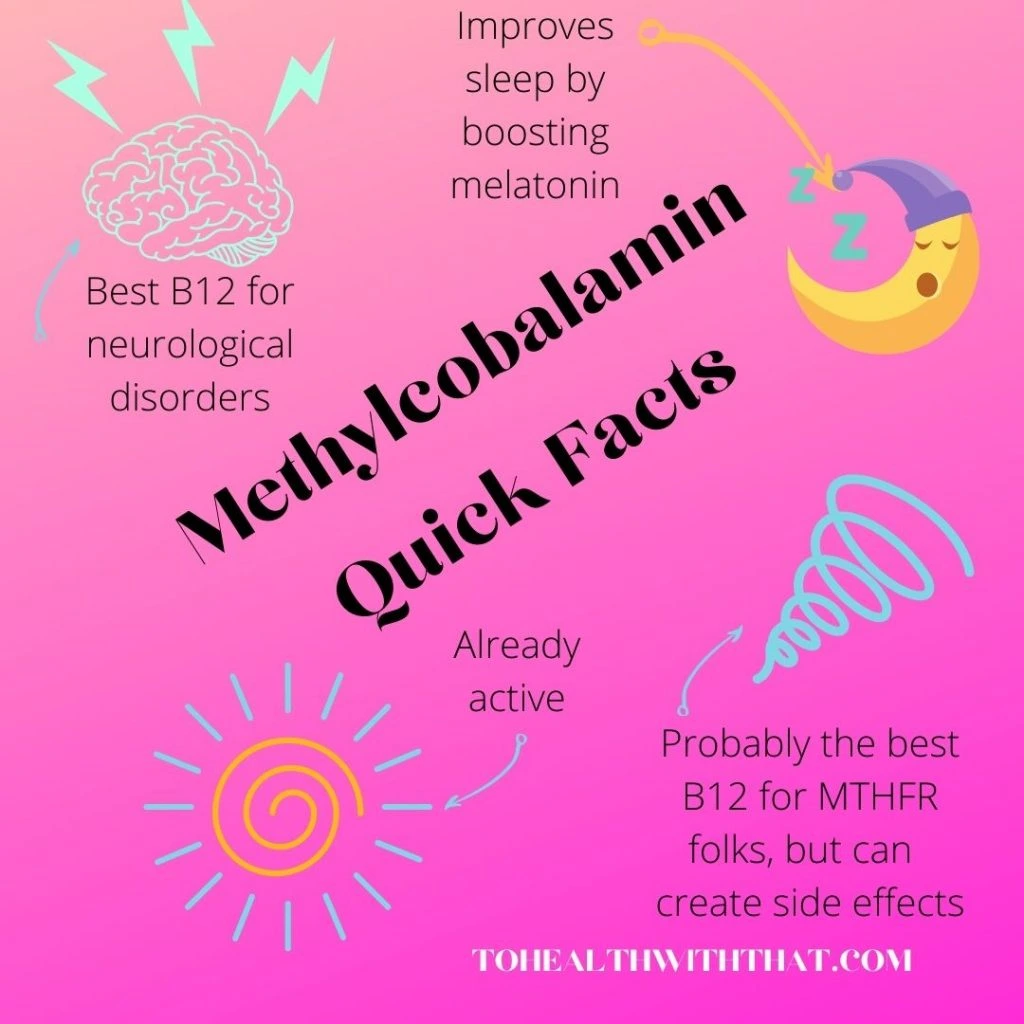
Methylcobalamin
Methylcobalamin is the active form of B12 and requires no interconversion to be used by your body. This is by far the best form for any issues involving degenerative neurological processes and can help relieve or reverse symptoms. It is a widely accepted adjunct therapy for peripheral neuropathy, Alzheimer’s dementia, Bell’s palsy, and other neurological disorders. It promotes growth, regeneration, and myelination of the nerves.
Methylcobalamin has also been studied along with adenosylcobalamin for anti-tumor effects and to inhibit the proliferation of various cancer cell types. Methylcobalamin helps to lower homocysteine levels and has even been used experimentally to inhibit the HIV-1 virus in human white blood cells. Additionally, methyl, the best B12 for MTHFR, may help with the methylation of serotonin to melatonin, your body’s sleep hormone and for some people, it improves sleep tremendously. Obviously, this form is a bit of a rock star.
For MTHFR folks, if you tolerate methylcobalamin, it’s a great choice, but some of us don’t tolerate the rapid absorption and rapid utilization. For people who have trouble, it can lead to feelings of anxiety, agitation, excitability, or insomnia.
Hydroxocobalamin
This is another inactive form of B12, and it is the form found most commonly in food sources. It is not bonded to anything toxic, the hydroxo group converts harmlessly to water. Compared to cyanocobalamin it bonds more easily to plasma protein and has a longer half-life in the blood.
When you take methylcobalamin and it uses its methyl group for something, it actually converts in the body to the hydroxocobalamin form, so these two interconvert easily, depending on whether or not they’re methylated. Taking the hydroxo form just means you need to use methyl donors to activate the B12, while taking the methyl form means it’s bringing its own methyl groups with it. Interestingly, hydroxocobalamin can scavenge nitric oxide, which is one of your body’s main vasodilators, and so it isn’t the best form for people with hypertension.
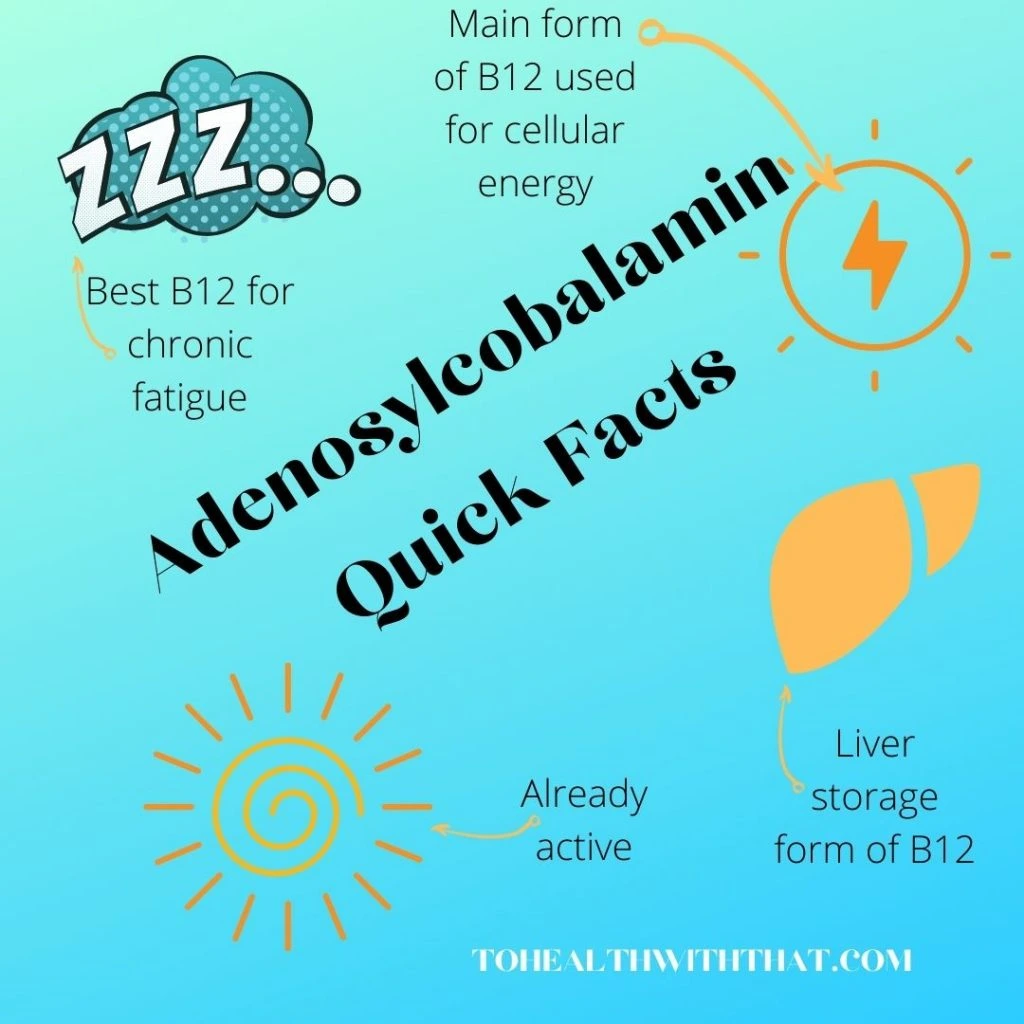
Adenosylcobalamin
Adenosylcobalamin is the other active form of B12, which is the predominant form that your body stores as B12 reserves in the liver. This is also the form that is used primarily in the mitochondria, which generate your cellular energy. Adenosyl is a great form especially in cases of people with liver issues.
There are some cases of chronic fatigue in which people only really feel better with adenosylcobalamin. They notice an increase in energy with this form but no other. This is thought to be due to a problem interconverting between the forms. If you notice a big difference with the adenosyl form it can be beneficial to look for a mixture of both adenosyl and methylcobalamin.
MTHFR is a common genetic mutation that can contribute to anxiety, depression, fatigue, chronic pain, infertility, and more serious conditions like breast implant illness, heart attack, stroke, chronic fatigue syndrome, and some types of cancer. If you know or suspect you have an MTHFR variant, schedule a free 15-minute meet-and-greet appointment with MTHFR expert Dr. Amy today.
Book Your Appointment

Hey Amy,
When you have B12 deficieny and take Methylfolate, you risk a methyltrap, because the B12 would normally take the Methyl part off of the Folate, right?
Now if I take Methylcobalamin, doesn’t the same thing happen? Because the B12 already got his own Methylgroup and doesnt use the Methyl part of the Methylfolate…?
I’m very confused right now, maybe you can bring some light into this question 🙂
Cheers
Hi Nils,
Yes – this part can be really confusing. So a methyl trap actually happens when there is a B12 deficiency because active folate is building up – you’ve got lots of that, but you don’t have the B12 that is necessary for the methyltransferase enzyme that would add a methyl group to homocysteine. So if you look at the methylation cycle and all of the other Bs that are necessary, it’s easy to see that the whole thing grinds to a halt pretty quickly if you don’t have the other Bs – I did a whole post about this here. If you look at the diagram in that post, you can see that B12 is a cofactor between the conversion from homocysteine back to methionine (which also uses a methyl group from 5-LMTHF). IF the B12 isn’t there, then the methyl group isn’t transferred and so 5-LMTHF builds up. If you’re taking B12 at all (of any kind) then this isn’t an issue unless you’ve been severely B12 deficient. If you’re taking methylcobalamin (methyl b12) then the B12 doesn’t need to use a methyl group from 5-LMTHF, which is what happens with the other forms of B12, because it already has its own.
So – the bottom line is that if you’re taking B12 and haven’t been severely deficient, then methyl trap isn’t an issue. It’s still important to take the other B vitamins as well because as you can see in the article I linked to above, they really are all necessary for any of this to work out. There is a lot of specific research on B12 and folate because the deficiencies mimic each other and are easy to confuse clinically, but all of the B vitamins are linked.
I’m not sure if I helped, or just made it more confusing. Let me know if you still have questions!
Hi Amy – methyl-mutant here,,
Glad to have stumbled upon this article as Ive been bewildered and befuddled on the topic of methylated B’s for a long time now..
Happily, you’ve managed to fill in a few pot-holes for me regarding Methylcobalamin and Methylfolate.
~ Not an easy task, I dare say.
Anyway, up until now, I’ve been using the Adenosyl/Hydroxy form out of fear of reacting, as I have been slammed with anxiety using nutritional yeast, and various B Complexes in the past.
I’m trying Methylcobalamin on for size right now – small doses – in hopes of being able to tolerate it.
Also, I’ve been using Folinic acid in place of MethylFolate for some time now, unaware of the fact that I needed to provide methyl donors for it.
I have multiple questions, but I’ll just trouble you with one of them right now. :/
~ Are SamE and TMG interchangeable as methyl donors for both inactive forms of Folate & Cobalamine?
Aloha & Mahalo from Hawaii,
Jeannine
Hi Jeannine,
I am SO glad you asked because this is actually kind of a sticky subject (also, can I come and see you in Hawaii some time because it’s on my bucket list?)
SAMe and TMG both look good on paper as methyl donors, but people seem to have very different reactions to them.
SAMe feeds directly into the methylation pathway and often pushes reactions in the same way methylfolate pushes reactions so if you try it, start low and go slow. It spins the same wheels that methylfolate does and so for some people it generates some of the same side effects.
TMG doesn’t push directly, but it still gives your body the methyl groups that it’s been missing and although it tends to be a little less reactive for folks than the SAMe, that doesn’t mean you should start with a flood. TMG will still generate some big changes in the way this cycle is able to operate so again start low and go slow.
I feel like I”ve just muddied the waters, so let me say it a different way. I feel like TMG is a great methyl donor if you’re able to take folinic acid and other forms of B12 without too much trouble. SAMe is more like a substitute or a work around for people who are truly folate intolerant, but it comes with some of the same pitfalls as methylfolate does so be careful with dosing.
Not sure if I helped there Jeannine, so follow up with more questions any time!
Good luck and keep us posted!