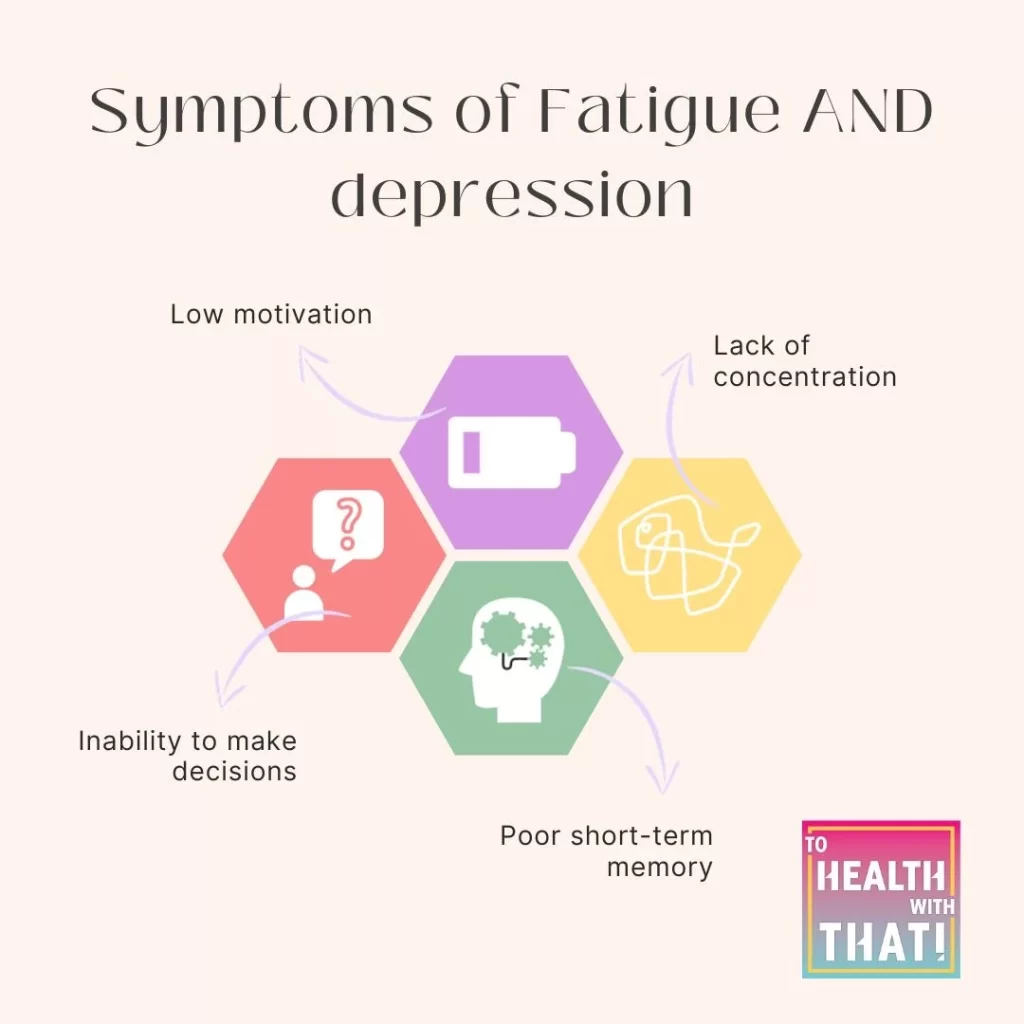
These two complex symptoms have a terrifyingly circular relationship, often blending seamlessly into each other, making it impossible to tell where one ends and the other begins. I have so many clients come to me with depression, but the symptoms aren’t sadness. It’s lack of energy, lack of motivation, lack of interest. It is depression, but it’s also fatigue. Lots of people who come in saying they are fatigued look exactly the same and many of them report an accompanying sadness or loss of interest because they’re just too tired to be bothered doing things.
Even for your doctor, it can be difficult to find the dividing line, and many people are being treated for one without truly addressing the other. Depression and fatigue dovetail into each other, and looking at them as two intermixed problems can be helpful in terms of finding solutions from different angles.
Why Fatigue Is a Symptom of Depression
We tend to think of the mind as one thing and the body as another, but the exciting thing is that the environment of your mind and your body are entirely intermixed. We think of depression as a neurotransmitter problem, but in reality, it’s bigger than that. Neurotransmitters are involved, but so are cytokines, inflammatory molecules, oxidative stress, and so much more.
The most common conventional drug-based therapies for depression center around neurotransmitters, but none of the other physiological changes are typically addressed. Some antidepressants, like desipramine and fluoxetine, do have anti-inflammatory activity, but it isn’t their primary focus.
In the first episode of this season, we talked about something called “sickness behavior,” which is the symptoms your body generates in response to a pathogen or major injury that essentially force you to act like a sick person and go to bed. In the context of a virus, this makes complete sense. You may have noticed, however, that depression and sickness behavior have a lot in common. It turns out, they have a lot in common on a molecular level as well.
Many of the cytokines, or signaling molecules, your body releases during sickness behavior are also elevated in depression, which helps account for the massive symptom overlap. Both states involve deep fatigue, listlessness, lack of interest in social activities, slower thinking, reduction of activity, exploration, and grooming, lack of enjoyment, and sleepiness. The fact that the chemistry of the two states is similar may give us new treatment targets for depression in the future.
Symptoms of depression that are not linked to these inflammatory cytokines include actual sadness, feelings of guilt or low self-esteem, and suicidal thoughts or ideation. Still, shared immuno-inflammatory pathways may underpin both states.
Why Depression is a Symptom of Fatigue
Fatigue by itself is also taxing to our mental and emotional health, possibly through the cytokines we mentioned before, but possibly also because feeling unable for long periods is actually crippling to the human psyche. It is easy to interpret your own lack of energy or clear-headedness as a personal failure. To feel guilty, unworthy, or sad because of it.
Sickness behavior does have the hallmark symptom of fever, which is not present in typical depression, although studies have shown that those with depression are likely to have higher resting body temperatures than those without, possibly due to the same inflammatory molecules
To make things more complicated, inflammatory cytokines have been shown to affect the levels of different neurotransmitters, including serotonin and norepinephrine.
Your Resting Normal Neurotransmitter Level
I believe there is a resting normal neurotransmitter level for most people that also influences this conversation, and that gene SNPs have a profound impact on that level. For example, many people, like myself, with slow COMT polymorphisms could be described as terminally cheerful. Depression in this group is likely to look very different from depression in a group with fast COMT function who tends to have lower resting neurotransmitters and less general chirpiness.
Resting normal neurotransmitter levels are part of the reason why I think so many people try antidepressants, go through the adjustment reaction, feel amazing for a few months, then slowly sink back to where they were. The natural consequence is to keep chasing that amazing feeling with dosage changes, medication changes, etc… but their body always seems to bring them back to their baseline eventually. For a more detailed discussion of why chasing neurotransmitters doesn’t often work, check out Season 1, Episode 49 or the linked blog post about neurotransmitters working as a web rather than a tug of war.
What You Can Do About Fatigue and Depression
It is all well and good to say fatigue and depression overlap significantly, but what do we actually do about it? Well, this is still a question, but research in this area gets nested under “treatment resistant depression,” which is what doctors call depression when antidepressants don’t work. Some of the therapeutic strategies for this include ketamine, which has become controversial because of its misuse as a street drug, and new drug candidates that are being researched that inhibit the glutamate, an excitatory neurotransmitter.
My own opinion, unbacked by research though it is, is that depression and fatigue treatments should also overlap, with some attention paid to both the inflammatory process in the body and mind as well as the changes to neurotransmitters.
Many natural substances that have shown promising effects for depression are also powerful antioxidants, which suggests they might also have effects on the inflammation and oxidative status of the body. Some of these include:
- Saffron – this bright yellow spice has been well documented for depression, but is also an incredibly potent antioxidant.
- Fish oils – Fish oils are a commonly used natural remedy for both depression and inflammation.
- Vitamin D – Low levels of vitamin D have been implicated in depression, and vitamin D has strong antioxidant function.
- St John’s Wort – This herbal medicine has long been used for depression, but studies show it also inhibits inflammatory signaling.
- Creatine – This common supplement for exercise performance and muscle development has also shown promise to reduce depression, inflammation, and oxidative stress.
- NAC – I have spoken a million times about the benefits of NAC as a precursor to glutathione, your master antioxidant, which therefore lowers inflammation and oxidative stress, but it is also a glutamate inhibitor, which means research is ongoing about the use of NAC for depression.
While I don’t suggest that you rush out and start taking all of these supplements, I do thin, it is important to consider your whole body in the treatment of depression, and your mind in the treatment of fatigue, and to potentially include some support that overlaps to both.
Research is also looking into novel drug therapies based on plant medicines or other existant drugs that don’t target the more conventional neurotransmitter pathways. I also want to mention some other therapies currently being researched.
Two of the studies currently ongoing are on plant medicines, including psilocybin from hallucinogenic mushrooms, and ayahuasca from the plant medicine of the same name. I have an enormous amount of respect for traditional plant medicines and have heard and witnessed incredible stories of transformation. These plant medicines have been used for centuries for people suffering from mental health disorders, spiritual and emotional crises, and grief, and even with our cultural fear of what we think of as recreational drugs, it is hard to deny their centuries of success.
Nitrous oxide, or laughing gas, is also being studied as a treatment for depression and is the subject of several ongoing phase I and II clinical trials. Remember, MTHFR folks, this one is not a great option for us because nitrous oxide is known to raise histamine levels sharply and can be dangerous with MTHFR.
Thank you so much for watching or listening today. Remember to like, subscribe, download, or make your offerings to appease the Youtube or podcast gremlins. I’d appreciate it.
MTHFR is a common genetic mutation that can contribute to anxiety, depression, fatigue, chronic pain, infertility, and more serious conditions like breast implant illness, heart attack, stroke, chronic fatigue syndrome, and some types of cancer. If you know or suspect you have an MTHFR variant, schedule a free 15-minute meet-and-greet appointment with MTHFR expert Dr. Amy today.
Book Your Appointment
